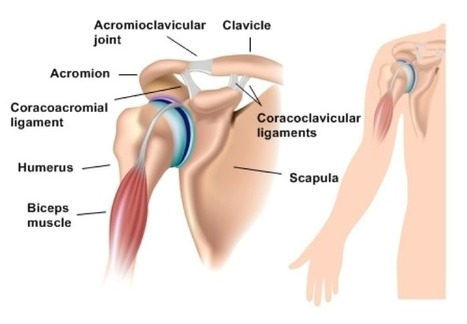
Dislocation of the shoulder joint is a common condition. The joint is unstable in comparison to many others. The shallow glenoid fossa and small articular surface in comparison of the head of the humerus produce an inherent weakness. The strength of the muscles and the capsule surrounding the joint are the main factors that maintain the stability of the joint.
Mechanism of Injury: Dislocation is produced mostly due to direct injury over the shoulder. Indirect violence following a fall on an outstretched hand can produce the same lesion. This can also happen inconclusive diseases like epilepsy, tetanus and following insulin shock therapy.
Types of Dislocation: The direction of the force of injury and position of the limb in relation to the trunk at the time of injury can displace the head of the humerus in different directions.
- Anterior dislocation: This is the commonest type and more than 90% belong to this variety. The head of the humerus is displaced anteriorly under the subcoracoid process.
- Posterior dislocation: This is an uncommon condition. The head of the humerus is displaced posteriorly.
- Inferior dislocation: This is the rarest variety in which the head is dislocated below the glenoid fossa. It occurs due to hyperabduction injury following a fall on an outstretched arm. The soft of the lower part of the joint is disrupted. The head of the humerus passes through this weak area and attains the infraglenoid position.
DIAGNOSIS
Clinical Features: Patient usually gives a history of falling on an outstretched hand and is unable to lift limb up. The affected side is supported by the normal limb. The contour of the shoulder is altered when compared with that of the normal one. There is prominence on the anterior part of the joint in anterior dislocation; gaping is characteristic below the acromion process in case of inferior dislocation and prominence can be felt and seen on the posterior aspect in posterior dislocation.
X-ray evidence: Radiological finding confirms the diagnosis. An x-ray should always be taken of both anteroposterior and lateral views. Appearance in one view may be deceptive. This is more so in posterior dislocation where only an anteroposterior x-ray has been taken. Evidence of any associated fracture should always be looked for.
TREATMENT
The dislocation is associated with injury to the soft tissue around the joint. Early diagnosis and reduction are essential. Failure to do these will lead to neurovascular complications involving the limb. Brachial plexus lesion with paralysis is common with delayed management.
Reduction: Some of the reduction can be done without anesthesia and most can be reduced easily under general anesthesia. Open reduction is needed only rarely in which surgery must be performed. But when open reduction is needed the orthopedic surgeons need to contact top orthopedic implant companies in India to obtain medical implants to perform the surgery.
REDUCTION OF ANTERIOR DISLOCATIONS
Several techniques of which Kocher’s and Hippocratic methods are the most popular have been adopted.
1. Kocher’s method: General anesthesia and the use of muscle relaxants are ideal. The surgeon holds the patient’s elbow with one hand and the wrist with the other.
Reduction is performed in four stages:
- Stage of traction– With the elbow in a flexed position, traction is applied on the arm of the patient.
- Lateral rotation– The forearm is laterally rotated while traction is maintained.
- Adduction: The arm is adducted by bringing the elbow towards the midline of the patient’s body.
- Internal rotation- The limb is rotated internally by bringing the hand of the affected side on the opposite shoulder. During this procedure, the head of the humerus is felt to be reduced.
2. Hippocratic method: This is done under general anesthesia. The patient lies on his back during the time of reduction. The surgeon exerts traction on the affected limb. The right heel of the surgeon is applied in the axilla for right shoulder dislocation where the left one for the left shoulder lesion. The foot is used as a fulcrum between the arm and chest wall of the patient. The traction is maintained while the limb is moved medially. This tends to replace the head of the humerus into its normal position.
Technique without anesthesia
- The patient sits on the chair in a sidewise direction. The upper margin of the backrest is covered with a towel or cloth over which the axilla of the patient rests. The surgeon holds the patient’s wrist with one hand and with the other holds the arm above the elbow. Gentle traction downward on the arm is maintained and the dislocation is reduced.
- The patient lies supine on the table with the affected limb hanging from the side of the table. Traction on the limb is applied by tying about twenty pounds of weight to the forearm. The reduction may take place slowly within ten minutes.
REDUCTION OF POSTERIOR DISLOCATION
The procedure is done under general anesthesia in four stages:
- Traction: Traction on the arm is applied.
- Adduction: Adduction of the limb is done while traction is maintained.
- External rotation: The forearm is externally rotated.
- Internal rotation: The limb is then internally rotated and the dislocation is reduced.
REDUCTION OF INFERIOR DISLOCATION
TECHNIQUE OF REDUCTION
This is done in two stages.
- Traction is an abduction. The affected limb is fully abducted and traction is applied upward in the direction of the long axis of the trunk. Counter-traction is applied by the assistant. This brings the head of the humerus in position with the glenoid fossa.
- Gentle adduction of the limb is then done and full reduction is obtained.
AFTER TREATMENT
Check for nerve lesion. Once the patient recovers from the anesthesia, the examination is made for any nerve lesion. Circumflex nerve damage is the commonest condition seen after shoulder dislocation. The deltoid function is tested by asking the patient to abduct the shoulder. Abduction may be absent also in associated rupture of the supraspinatus muscle is intact and there is no impairment of sensation over the outer surface of the shoulder. Abduction splint is applied in circumflex nerve and supraspinatus muscle lesions.
X-ray check-up– Post reduction x-ray must be taken in anteroposterior and lateral views.
Immobilization- This is to prevent recurrent dislocation, which is more common in young adults but rarely seen after the age of 50 years. In the younger group, the arm is immobilized in a triangular bandage for a period of 3 weeks. Patients with a previous history of dislocation should have the arm bandaged by the side of the trunk in adduction and internal rotation. Exercise is started after the period of immobilization.
COMPLICATIONS
- Nerve Injury: Circumflex nerve injury has been described. Most lesions are due to neuropraxia and improve slowly in abduction splint.
- Muscle Injury:
- Supraspinatus tear- The patient experiences pain and weakness during the abduction movement of the shoulder. Abduction splint is applied for 6 weeks.
- Biceps tendon: Dislocation of the biceps tendon from the bicipital groove may interfere with the process of reduction. The operative measure may be required in this condition.
- Recurrent Dislocation: Recurrent dislocation may be disabling and will need surgical repair in the future.
- Bony Injury:
- Fractures of the greater tuberosity- The fractured segment comes into normal position once the dislocation is reduced.
- Fracture of the neck of humerus along with dislocation-
This should be reduced by the closed method by the usual procedure. Failure to do this will require an open reduction. In elderly patients, the operation may be deferred and the primary aim will be to obtain the maximum mobility of the joint.